Came across this short lecture on schizophrenia and the inflammation hypothesis. The author mentions three hypothesis for the causes of schizophrenia – elevated dopamine, glutamate receptor abnormalities, and inflammation. He also mentions the fact that autoimmune diseases can present with psychosis – lupus, Hashimoto’s encephalopathy, celiac disease, etc. It’s great to hear a professional acknowledging this fact, as not all doctors look into the link between psychiatric symptoms and autoimmune diseases.
Important notes from the lecture – some inflammation can be determined in a straightforward way by checking the C-reactive protein levels. Elevated levels of this substance increase the risk of schizophrenia onset. C-reactive protein levels are used to check for infection or chronic inflammatory disease, they also lead to increased risk of heart disease. It can be elevated due to a variety of diseases, such as obstructive sleep apnea, some viral infections, lupus, and rheumatoid arthritis.
In one study lumbar puncture was performed on a sample of patients with schizophrenia. 54% of the patients had self-directed antibodies in the cerebrospinal fluid (another piece of evidence to support the immune system disturbance hypothesis). What could the antibodies be targeting? Possibly neuronal proteins or neuronal receptor proteins.
Tag: inflammation
Dr. Roger McIntyre: Mood Disorders and Metabolic-Inflammatory Comorbidity
Very interesting lecture found on YouTube – Dr. Roger McIntyre is a quite important guy in psychiatry here in Toronto. He is a Professor of Psychiatry and Pharmacology at the University of Toronto and Head of the Mood Disorders Psychopharmacology at UHN. He is also the director of the first Ketamine Infusion Therapy Clinic for depression in the GTA.
So in this lecture, which was posted in 2016, he talked about how just elevated C-reactive protein, a sign of general inflamamtion in the body, leads to anhedonia (inability to feel pleasure), apathy, and destuction in the brain of dopamine neurons. I wish more psychiatrists would actually listen to his lectures as well. I got a feeling, from personal experience, that some psychiatrists weren’t aware about the link between inflammaion and anhedonia, because they easily prescribed antipsychotics that cause severe weight gain. Dr. McIntyre actually speaks in the lecture against easily prescribing antipsychotics for depression, as weight gain is known to increase inflammation and therefore actually cause anhedonia/dysphoria.
So basically when an antipsychotic is described for depression – the antipsychotic reduces dopamine, since that is its function, and then further you can have death of dopamine neurons through inflammation, so that can result in complete dysphoria.
Prospective studies revealed that the average weight gain during the first year of treatment was 11.7 to 13.9 lb for clozapine, 15 to 26 lb for olanzapine, 4.4 to 5.1 lb for risperidone, 6.1 to 13.3 lb for quetiapine, and less than 2 lb for aripiprazole and ziprasidone.
Dr. Roger McIntyre: Mood Disorders and Metabolic-Inflammatory Comorbidity
Planks, gut health, and mental health
I’ve had many conflicts with my father, but one thing I’ve always agreed with him on is that there is no mental health without physical exercise. Especially for those with emotional instability like me, I find that exercise is a necessity. It’s definitely not easy to do it with an autoimmune disease since sometimes after I get home from work – I feel lethargic, or I feel arm pain, or I feel isolated and a need to go on Facebook and see that people are alive. Well this is where logical thinking comes in – in the end choosing to exercise has the best payoff even though it’s not immediate. Lying down on the sofa and turning on Netflix has an immediate pay off, but if this is what I will do daily after work, after a while I will be worse off.
Currently I am trying to exercise two to three times a day. I do about 10-12 minutes before leaving for work in the morning, I include stretching, planks, downward dog, inversion poses, etc. Recently there have been some articles about positive impact of even very short intervals of exercise. I would like to believe that these statements are true as I am not able to force myself to wake up another twenty minutes earlier and engage in a 30 minute work out before work or breakfast. I do believe that some exercise is better than no exercise. I work in a boring office, so my hours are pretty standard. During lunch I walk around listening to a podcast and currently I signed up at a yoga studio located in the office building downstairs, which offers lunch classes. In the evening I try to do another 20-30 minutes of exercise. Is this exercise plan difficult? Yes, but once you do it several days in a row, I feel that there is some kind of adjustment and you get used to the schedule. Also I find it easier when I know that my exercise interval is only 12 or 20 minutes, I am not trying to push myself into an hour jog. In fact I don’t jog at all. I mentioned this before – one psychiatrist with whom I had a consultation stated that the best way to combat inflammation is exercise and that I should only do the type of exercise that I like, otherwise I will not stick with the routine for long. Therefore no jogging for me, I am doing planks and yoga poses.
“The latest research shows that a single 10-minute bout of very light (30% of VO2 Max) physical activity can increase the connectivity between brain regions linked to memory formation and storage.
This potentially groundbreaking study on the cognitive benefits of short periods of mild exertion activity (such as gentle yoga, tai chi, slow dancing, or playing bocce) was conducted by researchers at the University of California, Irvine (UCI) and the University of Tsukuba in Japan.“
Ten minutes of mild exercise may improve brain connectivity and enhance memory
From the abstract of the actual paper: ” A single 10-min bout of very light-intensity exercise (30%V˙O2peak) results in rapid enhancement in pattern separation and an increase in functional connectivity between hippocampal DG/CA3 and cortical regions (i.e., parahippocampal, angular, and fusiform gyri). Importantly, the magnitude of the enhanced functional connectivity predicted the extent of memory improvement at an individual subject level. These results suggest that brief, very light exercise rapidly enhances hippocampal memory function, possibly by increasing DG/CA3−neocortical functional connectivity.“
Rapid stimulation of human dentate gyrus function with acute mild exercise
I now have some evidence to support my belief that my 10 minute work-outs are useful. Sometimes at work I do yoga poses in the staircase, or run up ten flights of stairs. There are many ways to exercise for free, it’s not necessary to purchase a monthly gym membership or pay $20 for a yoga class.
Some studies also indicate that exercise positively modifies gut bacteria. This change in turn can reduce inflammation and depression.
“Recent studies suggest that exercise can enhance the number of beneficial microbial species, enrich the microflora diversity, and improve the development of commensal bacteria.
Collectively, the available data strongly support that, in addition to other well-known internal and external factors, exercise appears to be an environmental factor that can determine changes in the qualitative and quantitative gut microbial composition with possible benefits for the host. In fact, stable and enriched microflora diversity is indispensable to the homeostasis and normal gut physiology contributing also to suitable signaling along the brain-gut axis and to the healthy status of the individual. Exercise is able to enrich the microflora diversity; to improve the Bacteroidetes-Firmicutes ratio which could potentially contribute to reducing weight, obesity-associated pathologies, and gastrointestinal disorders; to stimulate the proliferation of bacteria which can modulate mucosal immunity and improve barrier functions, resulting in reduction in the incidence of obesity and metabolic diseases; and to stimulate bacteria capable of producing substances that protect against gastrointestinal disorders and colon cancer (such as, SCFAs). “
Exercise Modifies the Gut Microbiota with Positive Health Effects
From ScienceDaily – “Two studies — one in mice and the other in human subjects — offer the first definitive evidence that exercise alone can change the composition of microbes in the gut. The studies were designed to isolate exercise-induced changes from other factors — such as diet or antibiotic use — that might alter the intestinal microbiota.”
Exercise changes gut microbial composition independent of diet, team reports
I think it’s very crucial to our mental health to exercise daily in any way – on a yoga mat at house, running up the stairs at work, going out for a jog, dancing, playing ping-pong, jogging with your dog, anything really that replaces sitting.
Tracking Anti-TPO and Anti-Tg antibodies
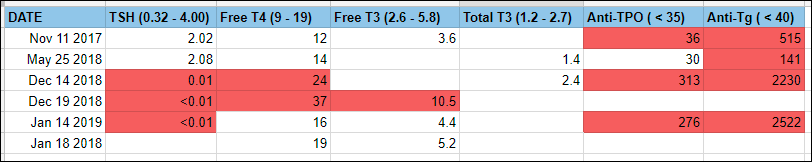
I have been tracking my thyroid antibody levels and I want to share my results, in case this information will be of use to someone. I have been diagnosed with Hashimoto’s encephalopathy in April 2017 and I was treated with intra-venous steroids (IV Solu-Medrol) in December 2017. In November 2017, before the steroids treatment, my thyroid hormone levels were normal, but my Anti-Tg and Anti-TPO antibodies were elevated. I was experiencing many symptoms such as fear, a sense of dread, severe anxiety, feeling of worthlessness. After the immunosuppressant treatment with steroids I had improvements in different areas of being, such as a desire to read fiction again, new interest in men, increased self-confidence, desire to play violin again. As you can see from the table below, my antibody levels decreased after the treatment, in May 2018 they were lower than in November 2017.
I was improving in 2018 – I started this blog, took a violin lesson, read sci-fi. In the fall I completed mandatory adoption training and started the homestudy process with a social worker for adoption of children. This is something that I want to do because I wanted to have a family for a while, but I don’t feel that passing on my genes is the right way, as likely my children would inherit the same autoimmune disorders.
In November 2018 I started feeling worse. It’s difficult to pinpoint a specific cause of this as there were several events. I have been gluten-free now since 2016. Unfortunately one day in November I ate a whole bowl of lentil soup with barley because the take-out place stated that the soup only contains lentils and rice. Such large amount of gluten after not eating it at all for several years could have caused an immune reaction. I also got the flu twice, and the flu can also lead to the immune system being overactive even after the virus is gone. I also decided to try different probiotic supplements which had supporting evidence in regards to positive results for mood improvement. Maybe it did not go well for me and these bacterial strains were not accepted by my immune system.
In end of November I started to frequently wake up around 5am covered in sweat. At work my palms were sweating and I was getting chills. My pulse was regularly over 90 and my temperature was around 37.3 Celcius even though I did not have a flu nor a cold. My neck and face were burning, I felt waves of heat and shivers going through my body. After work by 6 pm I was lethargic and couldn’t get myself to exercise as I was in the fall. It was very clear to me that my thyroid hormones should be tested, so I right away went to the lab. December results show that at that point my TSH was already very low because my thyroid hormones were too high. Thyroid antibodies are also elevated. Ultrasound confirmed inflammation of the thyroid. I was referred to Women’s College Hospital and they repeated blood tests again. It can be seen that December 19th results indicate even higher thyroid hormone levels.
At the moment when all this occurred, I had a regular schedule – sleeping 12am to 8am, working 9 to 5, was doing yoga before I became lethargic. I was not on any medications but I was taking several probiotic supplements – saccharomyces boulardii, and two probiotics for mood. I decided to stop all supplements and also came across an article about anti-Saccharomyces cerevisiae antibodies. I did not have testing for these antibodies, but I decided to try going yeast-free and see whether symptoms improve. I stopped drinking my kefir and eating my sourdough bread. Also avoiding alcohol and vinegar. It’s interesting to see that in January my thyroid hormones were at their normal levels. It’s hard to say whether there was an issue with the supplements that I was taking, or yeast in food, or a random event of thyroid inflammation. I will be testing again at the end of January. There is not much evidence that yeast consumption could cause an autoimmune flare, but I will still keep going yeast free for sometime to see whether there will be improvements.
“The findings indicate that ASCA IgG-positivity may be linked to the generalized inflammation commonly seen with increased adiposity, but not to dietary yeast intake. Other potential causes for the raised ASCA IgG concentrations, such as genetic predisposition, deviations in the gut microbiota and cross-reactivity of ASCA with other antigens, were not explored.”
Sourdough for mood and hyperglycemia
Not all carbs are equal. Several months ago I made a discovery of gluten-free sourdough recipes and now I eat it almost daily. I obtained a sourdough starter, and now that I have one, it can live on forever, as long as it gets fed. It can definitely outlive me! Feeding the starter is very simple and requires only two ingredients – brown rice flour and warm water. After being on a strict AIP diet for almost a year (a lot of food group exclusions, including grains), it was very exciting to once again eat bread, burritos, and blueberry muffins. I no longer follow the strict AIP diet since it did not turn out to be a magical cure for me. I did improve a bit, but that does not mean that every food group exclusion contributed to my improvement. One person (me) trying the AIP diet is not a clinical trial with test and control groups.
I do see strong correlation between my psychotic episodes and consumption of gluten/cow’s dairy/corn/chocolate/nightshades (bell peppers are fine, small amounts of tomatoes are also OK)/ high-glycemic foods. I haven’t found issues with eating gluten-free whole grains and also found no evidence that grains are inflammatory. I don’t consider any blog post evidence. If a blog post refers to a research paper, then I will consider their claim. I do agree that anecdotal evidence is also useful, it was other people’s stories that helped me to obtain the right diagnosis after being misdiagnosed with schizophrenia by my psychiatrist. Only we can’t know from anecdotes what actually helped, if someone did the AIP diet and they got better – was it because they eliminated all the foods the diet suggests to exclude, or they could have improved just as well if they only avoided refined carbohydrates?
The evidence that I found so far indicated that whole grains are actually anti-inflammatory. For example, whole grain intake was found to be inversely related with inflammatory protein concentrations, while refined grain intake was positively related with the inflammatory markers. “In summary, whole grain intake was inversely related to PAI-1 and CRP plasma concentrations, but these relationships were attenuated by the addition of metabolic variables to the model. Refined grain intake was positively independently related to plasma PAI-1 concentrations.“
Whole and Refined Grain Intakes Are Related to Inflammatory Protein Concentrations in Human Plasma
I introduced whole grains after a year of strict AIP diet with no problem. I find that consumption of whole grains puts me in a more relaxed state of mind, I actually consume half a cup of rolled oats with green banana flour in the evening for better sleep. Sourdough is great because the baked goods end up with a low glycemic index after the fermentation process. I have a glucometer that I use to determine my blood glucose response to different food products. The standard test is a two-hour glucose test. Two slices of gluten-free bread increased my blood sugar to over 11 mmol/L two hours after consumption, which is a sign of high blood sugar. I did the same test with sourdough bread and sourdough muffins and my blood sugar was back to under 6 mmol/L two hours after consumption, which is a big difference. Short grain brown rice is also a high glycemic index food, while long grain brown rice was found to have lower glycemic index.
Sourdough allows me to eat the foods that I missed out on for so long, at the same time it does not cause a blood glucose spike for me. I have used sourdough to make pizza crust, tortillas, bread, and muffins. Currently I am learning to use fermented batter to cook dosas, an Indian dish. Controlling blood sugar for me means also stabilizing my mood. A glucose spike and then crash turns me lethargic and weepy, it takes away my energy, I definitely want to avoid that. Sourdough allows me to have blueberry muffins for breakfast, goat cheese toast, burritos – all without the consequences of an emotional roller coaster. High glycemic foods may also promote inflammation and given my diagnosis of autoimmune encephalitis, that is something that I definitely want to avoid as well.
“Hyperglycemia can cause inflammation through varying mechanisms that result in the production of free radicals and pro-inflammatory cytokines (19, 24). Thus, high glycemic index and glycemic load diets may stimulate inflammation. Glycemic index is the blood glucose-raising potential of the carbohydrates in different foods. A more accurate indicator of the relative glycemic response to dietary carbohydrates, however, is glycemic load. Glycemic load incorporates the relative quality of carbohydrates characterized by the glycemic index. Consumption of high-glycemic index foods results in higher and more rapid increases in blood glucose levels than the consumption of low-glycemic index foods. Rapid increases in blood glucose are potent signals to the β-cells of the pancreas to increase insulin secretion, which can cause a sharp decrease in glucose levels and lead to hypoglycemia (25). In contrast, the consumption of low-glycemic index foods results in lower but more sustained increases in blood glucose and lower insulin demands on pancreatic β-cells (26).“
Dietary carbohydrates and inflammation

Are you sure your depression is in your brain?
I’m not. Actually I’m pretty sure that’s not where my depression started. I am quite positive that the encephalitis – brain inflammation – had developed after several years of chronic gut inflammation. What if my irritable bowel/gastritis was stopped right after it started? What if I had known about celiac disease and stopped eating gluten not two, but ten years ago? My assumption is that I would not have developed brain inflammation then, I would not experience seeing the old women asking me to help them die, I would not feel the walls of my room closing in on me. There would be no primal fear, no encephalitis. Whatever has happened to me, happened, no point to dwell on the past, but I am writing for others, for whom such terrifying experiences may be prevented. It’s important to ask the question – are you sure your depression is only in your brain?
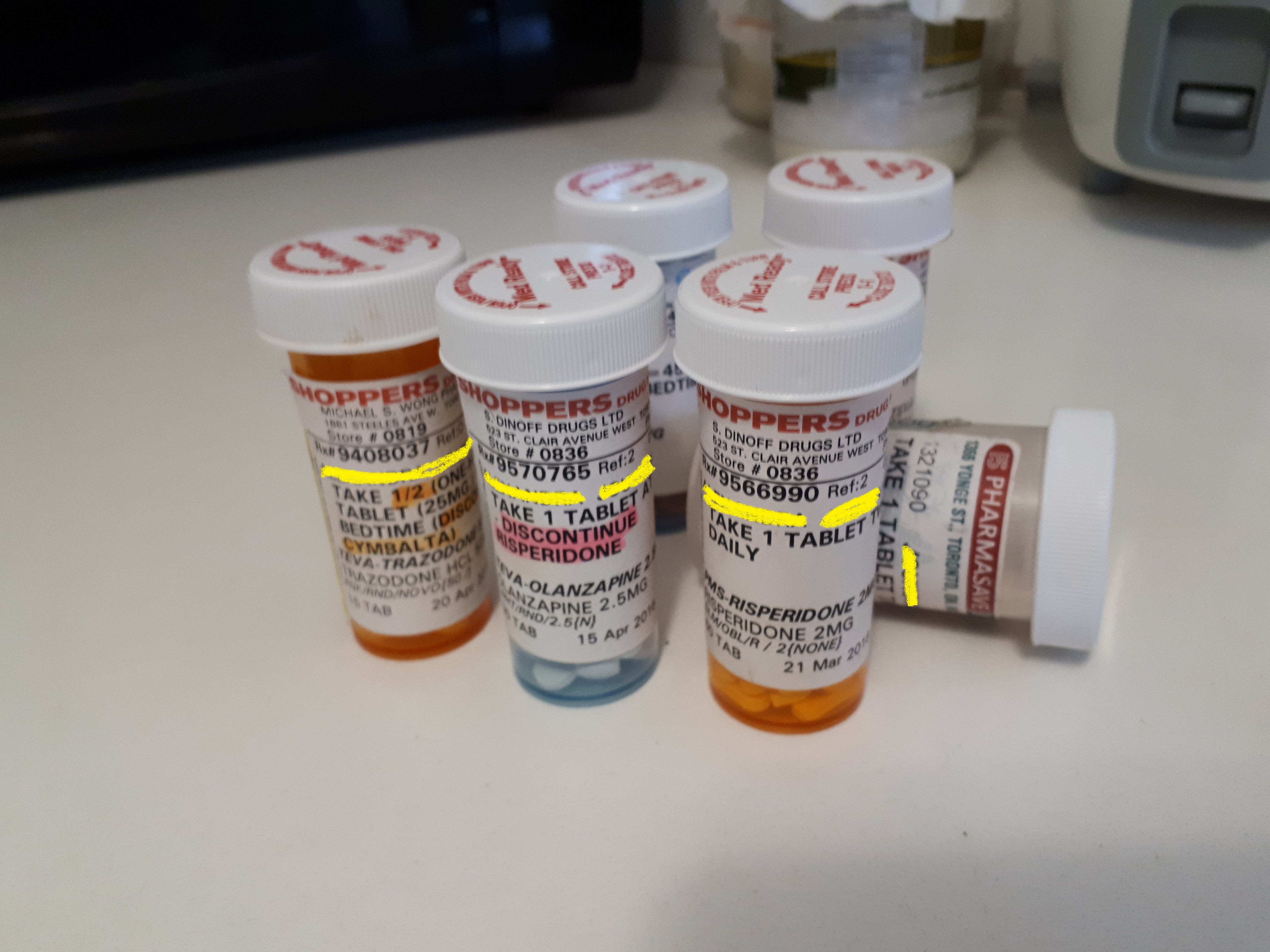
Above is my combination of the psychiatric meds that I was given by my first psychiatrist. She never questioned the origins of my depression – to her it was all a chemical imbalance in my brain, therefore she combined SSRIs, antipsychotics, benzodiazapines, and she failed at treating me. She started treating me in November 2015 and in May 2016 I bought hibachi grills and drove away into a forest with the two grills and a bag of charcoal, police had to track me. In June I could no longer work and became unemployed. Clearly I did not improve in the six months that I was her patient.
I did not improve because I don’t just have some serotonin imbalance, I have autoimmune encephalitis – brain inflammation. I also was diagnosed previously with irritable bowel syndrome (IBS) and chronic gastritis – gut inflammation. Did one lead to another? I believe so. I believe my depression started in the gut and there is research to support this theory.
“Recently, studies have emerged focusing on variations in the microbiome and the effect on various CNS disorders, including, but not limited to anxiety, depressive disorders, schizophrenia, and autism.2,8,9 Therapeutic interventions to treat dysbiosis, or disturbance in the gut, and mitigate its effects on the GBA (gut-brain axis) are only recently coming to the forefront as more is known about this unique relationship. As a result, research has been done on the use of probiotics in treatment of anxiety and depression both as standalone therapy and as adjunct to commonly prescribed medications.”
“When the human microbiome is challenged with changes in diet, stress, or antibiotics, the physiology of the normal microbiome undergoes change. A dysbiotic state leads to increased intestinal permeability and allows contents such as bacterial metabolites and molecules as well as bacteria themselves to leak through the submucosa and into the systemic circulation, a phenomenon aptly named leaky gut syndrome. … Increased intestinal permeability leads to detrimental effects on the host immune system, which have been demonstrated in diseases such as inflammatory bowel disease (IBD), diabetes, asthma, and psychiatric disorders including depression, anxiety, and autism.2,4,10,34,35“
“Depressive disorders are characterized by both neuroplastic, organizational changes, and neurochemical dysfunction.42 Illness is thought to begin when there is deregulation of these systems and can largely be attributed to cytokine release secondary to an exaggerated systemic response to stressors.39,41 Endotoxin infusions to healthy subjects with no history of depressive disorders triggered cytokine release and subsequent emergence of classical depressive symptoms. The study established a direct correlation between increased levels of IL-6 and TNF-a with symptoms of depression and anxiety,43 indicating that pro-inflammatory cytokines play a role in the development of anxiety and depression. These effects correlated with a state of chronic inflammation and altered immune cells in the peripheral blood. However, TNF-a administered to healthy subjects resulted in no depressive symptoms,38 suggesting that toxin induced inflammation caused the mood disturbance.”
Gut microbiota’s effect on mental health: The gut-brain axis
There has also been found a link between IBS and depression and recent studies are indicating that probiotics may help with both issues.
“For the new research, scientists from McMaster University in Canada recruited 44 adults with IBS as well as mild to moderate anxiety or depression. They were followed for 10 weeks; half took a daily dose of the probiotic Bifidobacterium longum, and half took a placebo. The probiotics were manufactured and provided by Nestle, which also funded the study. (Nestle was not involved in collection, analysis or interpretation of study data.)
After six weeks, twice as many people who took the probiotic had decreased depression scores compared to those who took the placebo: 64% versus 32%. Results were similar after 10 weeks, as well. When people in the study were given functional MRI scans, the researchers found that improved depression scores were associated with changes in activity of several brain areas involved in mood regulation.”
How Probiotics May Help Depression
If you are suffering from treatment resistant depression – you are not improving with the SSRIs/SNRIs/TCAs/MAOIs/NASSAs/etc., it’s important to ask yourself whether you are also suffering from any other conditions. If I had previously known all the information about the gut-brain axis, inflammation, and autoimmune diseases, it would be more evident to me that the cause of my psychiatric issues was likely gut inflammation. My severe depression started in 2015 but other health problems were starting long before that. I experienced dry and peeling skin since I was 11 years old and after the age of 12 I developed severe acne. When I was 17 I started having strong abdominal pain in the evenings. Sometimes the pain was so severe that I found it difficult to sit up. I also remember difficulties with falling asleep because as I lay down I would feel my stomach grumble and I could not relax. Later on more symptoms were added such as facial swelling, gastric pain, rapid weight gain, and brain fog. Then the depression and psychosis came. A coincidence ? Just a chemical imbalance unrelated to the other health issues? Clearly not and these symptoms were all related. They developed together as I continued to have a diet, unknowingly, that was terrible for me – pasta, bread, pizza, cheesecakes, and the symptoms declined together as I changed my diet, got treated with steroids, and started consuming fermented foods.
Now that I am equipped with all of this information I hope that I will continue to improve. I no longer have a feeling that it will only get worse and worse. I hope this will be useful to you as well and I hope I can help you feel happier again. There is more and more research now on other possible treatments for depression in addition to existing antidepressants, so I am optimistic that something will work for you, there are many things to try, don’t give up!
Yes, I am using this self-made incubator instead of Zoloft to treat depression
Here is my self-made incubator. It was constructed at home from several cheap and available components – a nice big Styrofoam cooler, a light bulb, a light bulb socket, a temperature controller, and some tape. That’s all, very simple. The cooler I got from Canadian Tire for about $14, light bulb, socket, and tape also from Canadian Tire. The temperature controller I purchased on Amazon for $35. What does the incubator do? The light bulb goes inside the cooler, so does the sensor from the controller. You close the lid and choose the desired temperature. The controller keeps the light bulb on until the chosen temperature is reached, then it turns it off. If the temperature drops, the light bulb is turned back on.

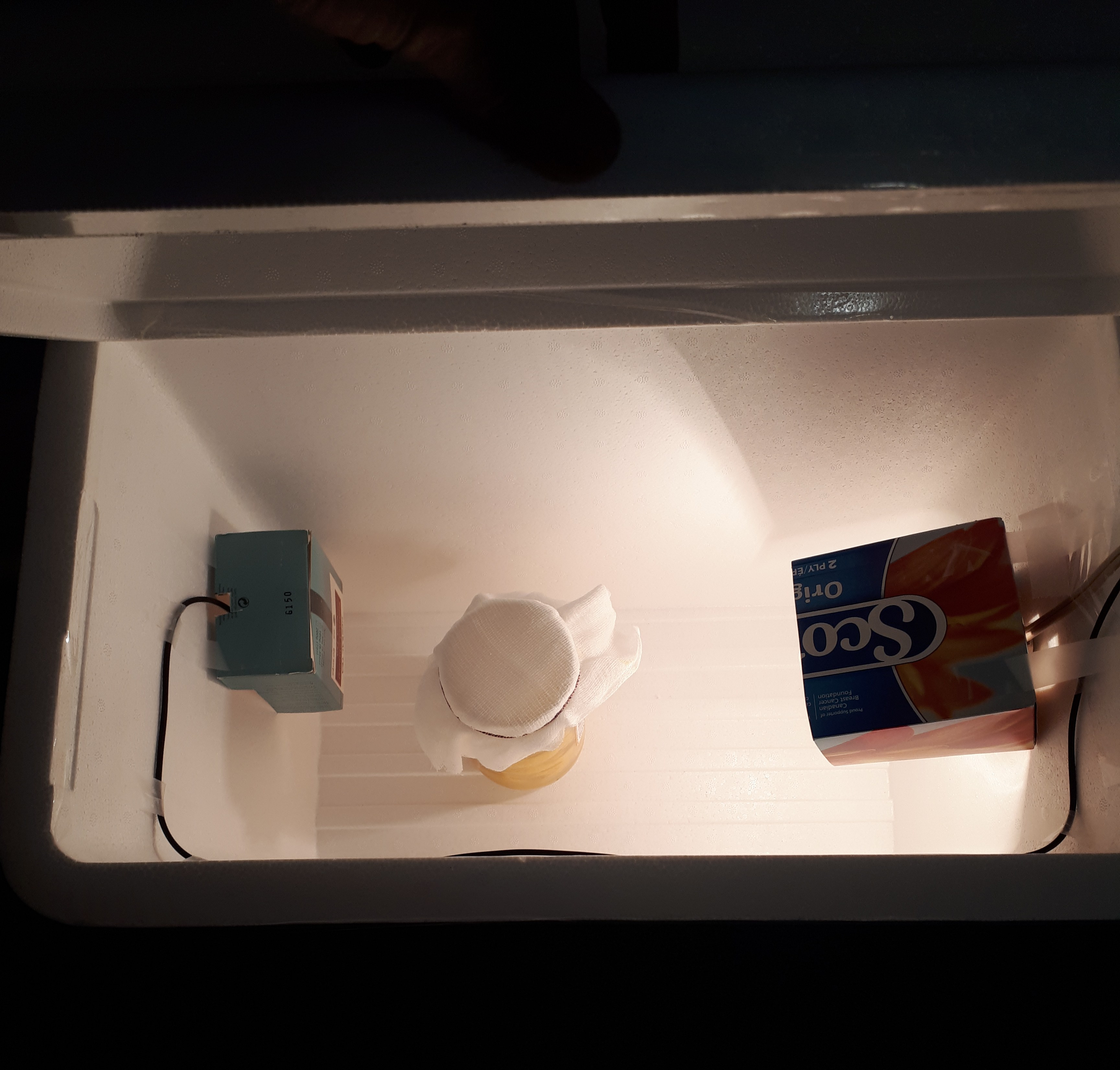
How is any of this relevant to depression treatment? Well turns out that it is, and this incubator has been helping me a lot more than my previous trials of anti-depressants. I use the incubator to make fermented foods and research shows that eating probiotic foods can reduce chronic inflammation in the body and this in turn can reduce symptoms of depression. I have been making goat kefir, goat yougurt, sourdough, fermented fruits. I have also ordered a tempeh starter – spores of a specific mold, Rhizopus, that is used to ferment soy beans. I have also been buying natto (another type of fermented soy beans) in a Japanese store and eating it for breakfast.
It has been a bit more than a month since I started all this fermented food consumption and I think it has definitely improved my brain function in many ways. Correlation doesn’t mean causation, but I have noticed improvement in the way I think, the way I react to stressful events, my ability to sit down and spend time on meditation. I have rediscovered my interest in violin playing and my interest in the opposite sex. Last week I found my headphones because I wanted to listen to David Guetta in the subway on my way to work. Maybe that doesn’t sound like much, but if you’ve experienced severe depression and if you’ve seriously considered suicide, I think you would understand that this means progress. If you have experienced a state of mind in which your only desire was finding a way to end your life, then you know that going to a state where you have a desire for something else, anything else, is definitely an improvement.
I think therefore that constructing this incubator was the best decision this year so far. Last year the best decision that I made was pursuing immunosuppressant with intravenous steroids. I was treated with IV Solu-Medrol for five days in December and after that I saw my mind opening up. No, my depression did not vanish, but I started to have ideas, to be more proactive. Participating. I through of sharing my experience with autoimmune encephalitis, so I started a blog. I took the psychiatrist’s advice to do aerobic exercise in order to reduce brain inflammation. I researched further anti-inflammatory treatments and decided to build an incubator. I also became interested in helminthic therapy, so I learned how to use bitcoin and purchased some helminth larvae in order to infect myself. I don’t think this is all a coincidence, I think the steroids treatment did reduce inflammation that was there in my brain and some neural pathways opened up, more ideas started coming in. My tunnel vision became broader, the world became less black and white.
You can read my previous post about fermented foods and depression treatment here:
Bacteria, yeast, stinky tofu, desire?
My case of severe depression and improvement after immunotherapy is another piece of evidence supporting the idea that depression and suicidal thoughts are not always just caused by imbalance of serotonin, but inflammation can also play an important role.
Recently researchers at the University of Manchester conducted a study measuring level of inflammation in the brains of patients with clinical depression. “Dr. Talbot and colleagues measured the levels of translocator protein (TSPO) in the brains of people diagnosed with major depressive disorder. TSPO generally plays a role in the immune response system and cell death.
In the brain, elevated TSPO levels activate the microglia, which are immune cells specific to this organ. Microglial activation indicates brain inflammation, so this is what the scientists targeted.
People with depression who were experiencing suicidal thoughts were found to exhibit significantly higher levels of TSPO, associated with microglial activation and indicating inflammation of the brain.“
Depression: Is brain inflammation tied to suicidal thoughts?
I was suffering from treatment resistant depression, but now I believe that it is not resistant, the treatment was just incorrect. I was put on mirtazapine, bupropion, risperidone, sertraline, multiple combinations of antidepressants and antipsychotics were tried. Well none of those combinations worked, but today I am still alive. I cannot thank my psychiatrist who continued to treat me with the same medications just in different doses and mixes, but I am thankful to all the researchers, journalists, and bloggers, who have written on the topic of the link between inflammation, suicidality, and depression. I am very thankful for Susannah Cahalan for her book “Brain on Fire: My Month of Madness” about her terrifying experience with anti-NMDA receptor encephalitis. I think, maybe not in the average psychiatrist’s office, but in general there has been progress in understanding the impact of our diet, lifestyle, and chronic inflammatory conditions, on mental health. Diet matters, exercising matters, so does our gut microbiome, blood glucose levels, inflammatory markers. All of this cannot be fixed by just taking Zoloft or Prozac and I believe that is why many people don’t get better on antidepressants. They are not treatment resistant, the right treatment is available, it just hasn’t been applied.
Industrialization, autoimmune diseases, and depression
I used to think that I was in control of my own mind, but it’s clearly not the case. I don’t choose how to feel and how to emotionally respond to situations, just as I don’t choose when to feel hungry. I don’t choose my thoughts as well. I don’t know which thought is going to come next, it’s just going to pop up in my conscious mind and I will observe it, I will react to it. Someone recently told me that all the choice that we have in life is the direction of our view. We don’t choose our emotions, we don’t choose our thoughts, we don’t choose the environment around us, we can only turn our head and change the view, and observe.
That’s why doctors prescribe antidepressants – people don’t choose to be depressed and they can’t just “think their way out of it”. And sometimes antidepressants help, maybe for some people depression is just a lack of serotonin and SSRIs fix that imbalance. The chemical imbalance theory is not 100% confirmed, some scientists debate whether this is a cause of depression at all, perhaps antidepressants help some people not by increasing serotonin, but by decreasing inflammation. Autoimmune diseases are what can cause chronic inflammation. This is when “the immune system prompts white blood cells to attack nearby healthy tissues and organs, setting up a chronic inflammatory process”. Turns out the brain can be affected by this process as well. “People who had been treated for a severe infection were 62% more likely to have developed a mood disorder than those who never had one. An autoimmune disease increased the risk by 45%. Multiple infections or the combination of severe infection and an autoimmune disease boosted the odds of developing depression, bipolar disorder, or another mood disorder even further.”
Infection, autoimmune disease linked to depression
Next I am going to speculate and talk about the possible causes of rising incidence of autoimmune disease. I am going to mention the idea that the lifestyle that we obtained through industrialization turned out to be pro-inflammatory. I am not proposing to go back to living in a village, but I want to propose making practical lifestyle changes that can help reduce chronic inflammation and in turn depression.
We are participating in less physical activity and are gaining higher body weight
One result of industrialization is we are eating more sugar, moving less, and weighting more. “How could carrying extra weight and sofa-sitting be connected to higher levels of inflammatory chemicals in the body and the development of diabetes?
Researchers discovered that excess body fat, especially in the abdomen, causes continuous (chronic), low levels of abnormal inflammation that alters insulin’s action and contributes to the disease.
The body becomes less sensitive to insulin and the resulting insulin resistance also leads to inflammation. A vicious cycle can result, with more inflammation causing more insulin resistance and vice versa. Blood sugar levels creep higher and higher, eventually resulting in type 2 diabetes.“
Are Diabetes and Inflammation Connected?
We are eating high glycemic foods
We are eating more processed and high glycemic foods. The bread that people used to eat when they lived in villages was usually not the white bread from refined flour, it was sourdough, which has more nutrients, and a low glycemic index. I doubt anyone used to eat pasta, pizza, or fries often, if at all. I know that in peasant Russia there was fermented cabbage, sourdough rye bread, barley, and broth, sometimes meat and fish. Also fermented milk products. None of those foods have a high glycemic index.
“According to Harvard researchers, healthy, middle-aged women who ate the meals with the lowest glycemic load had the lowest levels of C-reactive protein, a marker of inflammation in the body.
In overweight women who had greater levels of C-reactive protein to begin with, eating higher amounts of low glycemic index foods had an even greater impact on their inflammatory markers.“
The Link between Glycemic Index, Diabetes, Inflammation and Heart Disease
We are eating fewer fermented foods
How often do you drink kefir or yougurt, eat kimchi or sauerkraut? Do you eat natto or fermented bean curd? Tempeh? Sourdough bread? Cassava fufu? If the answer is pretty often, I would say that’s good, but many people in US and Canada rarely eat fermented foods. Maybe sometimes yougurt, but it’s questionable whether store bought yougurt has live probiotics. Previously people ate fermented foods more often. They didn’t really have much choice since refrigerators weren’t available. Milk goes bad pretty quickly, so you need to make it into kefir or yougurt. In winter you don’t have fresh vegetables, you have fermented vegetables in jars that you prepared during the summer. Same with fruits. There have been several papers recently linking fermented foods to mental health, here is what is stated in one of them: “The extent to which traditional dietary items may mitigate inflammation and oxidative stress may be controlled, at least to some degree, by microbiota. It is our contention that properly controlled fermentation may often amplify the specific nutrient and phytochemical content of foods, the ultimate value of which may associated with mental health; furthermore, we also argue that the microbes (for example, Lactobacillus and Bifidobacteriaspecies) associated with fermented foods may also influence brain health via direct and indirect pathways.“
Fermented foods, microbiota, and mental health: ancient practice meets nutritional psychiatry
We have lost our “old friends”
One of recent theories is that the rise in autoimmune disorders could be due to our gut microbiome depletion. With sanitary toilets, pasteurized milk, less time with animals (urban citizens rarely hang out with farm animals, neither do they milk cows, and now few even have pets due to smaller apartment sizes), we have lost many microbes and parasites that used to inhabit our gut. Turns out this might not be a good thing. It could be that because we as species cohabited with these organisms for so long, our immune system evolved to train on these parasites, and now we are lacking this training. “Diminished exposure to immunoregulation-inducing Old Friends in the perinatal period may enhance the consequences of psychosocial stressors, which induce increased levels of inflammatory mediators, modulate the microbiota and increase the risk for developing all known psychiatric conditions. In later life, the detrimental effects of psychosocial stressors may be exaggerated when the stress occurs against a background of reduced immunoregulation, so that more inflammation (and therefore more psychiatric symptoms) result from any given level of psychosocial stress. This interaction between immunoregulatory deficits and psychosocial stressors may lead to reduced stress resilience in modern urban communities.“
Microbial ‘Old Friends’, immunoregulation and stress resilience
Do we need to move back to the village? Or to a cave?
Well I’m hopeful that I won’t have to, because my job is in downtown Toronto, and it would be hard to commute there from a remote village. I hope that given the recent research, we can use this information to improve our immune system function, while still living in a city. We can cook more food at home instead of buying processed food. I rarely buy anything at the food court during the work day, I bring everything from home. I am also making fermented foods – kefir, yougurt, sourdough bread, kombucha. I also purchased some at Asian grocery stores – they have fermented bean curd, natto, fermented Chinese cabbage.
In terms of moving around, I try not to sit at my desk at work for too long. I get up to make tea, go for a walk during lunch. Walk to the subway in the morning instead of taking the streetcar. Walk home after work with a friend. Gym I personally found very boring, but I do exercise at home with an aerobic step. Doctors suggest at least 30 minutes of aerobic exercise a day, heart rate needs to go up!
In terms of bringing back “old friends” – this can partly be done by consuming probiotic and prebiotic foods to increase gut microbiome diversity. There are also soil bacteria that are considered beneficial, we can obtain them by spending time near soil and breathing in the particles. Having a dog is stated to have beneficial effects on our gut microbiome. There is also experimental helminthic therapy – infecting yourself with parasites on purpose. I am planning on trying this therapy and I will write more on this topic later on.
Bacteria, yeast, stinky tofu, desire?
It has been now about three weeks that I started experimenting with kefir and fermented foods. I’ve been drinking kefir almost every day. Fermenting it every two days in a two-liter jar. I can easily drink one liter a day. I also made yougurt, using store-bought yougurt as a starter. Kefir and yougurt both from goat milk, as I mentioned previously – I don’t tolerate cow milk. What does it mean not tolerate? Well it gives me bad thoughts. Thoughts about people dying, about the meaninglessness of life. I don’t want those thoughts. Yes, correlation doesn’t mean causation, but I have this observed this increase in the intensity of negative thoughts after consuming milk so many times that it’s definitely worth it avoiding it. Also there are studies suggesting that there is a link between casein and immune response. Immune response could mean brain inflammation, it could mean psychosis. That is what I observe.
“Multiple studies have documented immune activation in individuals with schizophrenia. One antigen capable of inducing a prolonged immune response is bovine casein derived from ingested milk products. Increased levels of casein antibodies have been found in individuals with schizophrenia after diagnosis.”
Association between bovine casein antibody and new onset schizophrenia among US military personnel
So I have been consuming homemade kefir and yougurt. Currently brewing kombucha in a jar on my kitchen counter. I have also made a jar of probiotic apples and fermented a mango with yeast. I purchased an active dried yeast supplement, saccharomyces boulardii. I am trying to include all sorts of probiotics, yeasts too, not only bacteria. Bacteria and yeast are both single-celled organisms, both have cytoplasm and a membrane surrounded by a cell wall – that is what Google says. Yeast cells have a nucleus, while bacterial cells do not. Certain types of bacteria and yeast can survive in the human gut. There has been some research, and saccharomyces boulardii is supposedly one of those yeasts. It has been found to benefit patients with gastrointestinal diseases, it might improve the gut microflora. I took it in capsules that it is provided in, as well as opened one capsule into my mango jar and let it stand for two days. The taste has come out quite strong, but I don’t think it has gone bad, I did not get any stomach ache after consuming the fermented mango. Was not great for my taste buds, I might try adding some honey next time for fermentation, but my combination of consuming yeasts and bacteria from kefir, yougurt, kombucha, and fermented foods, I think had a positive effect on my mind.
One change that occurred was after two weeks of daily kefir consumption. I suddenly had a desire to play my violin, which I haven’t touched in six years. Ever since moving to Waterloo for grad school in 2012 and later on becoming depressed, I have abandoned my violin practice. After I was already out of school and had free time after work, I just had no desire to play. All music was emotionally painful for me. Also I felt that it was pointless – I started learning at 19 years of age, that it top late, I thought, I would never learn to play well. Therefore the violin had been abandoned and was lying silently in its case at my parents’ house.
Last week though, when the desire to play occurred, I did not have any of these doubting thoughts such as what is the point of playing, would I be able to learn. I just wanted to play again and that is what I did. And that is beautiful, this experience of undoubting desire, this is something that depression completely takes away from you. Depression is not wanting things that are part of this world, not enjoying them, having no desire. Only the wish for your experience in this world yo end. So was that occurrence a coincidence? I don’t think so. I don’t think desire suddenly appears after six years of absence without any chemical changes. I think the bacteria and the yeast in kefir had something to do with it.
“It’s been known for some time that one’s gastrointestinal tract functions in essence as one’s “second brain”, lined with hundreds of millions of neurons. In fact, the gut manufactures more dopamine and serotonin, important neurotransmitters that powerfully influence mood and motivation, than does the “head” brain.”
A Gut Feeling: Probiotics and Changes in Brain Activity
On Sunday there was a second event. I have to mentioned that ever since I got severely depressed, I gradually lost desire for anything. Playing violin was one of activities that I stopped. I stopped reading for please. Stopped writing in my livejournal. Everything seemed pointless, all activities fruitless. We are all going to die anyways and become nothing. I think last time I had my own idea was in summer of 2015 – I was very frustrated with Toronto’s public transit system and I decided to make an electric longboard. I succeed and it actually still works. After that I don’t remember pursuing any interests, my days were overwhelmed with feelings of intense fear, loneliness, sadness. Probably my brain inflammation intensified at that time, that is when I first got involuntarily hospitalized in a psychiatric unit. So having something to be exited about, a longing for an activity – I find that a dramatic improvement. No desire for me means no interest in life, desire is willingness to live.
The event then was that I suddenly found someone attractive. That hasn’t happened to me in years. Depression is loss of all pleasures. A loss of pleasure in reading, in traveling, in sex – in whatever you used to do. Attraction is the opposite, attraction is desire. So yes, for me it was a big deal. It felt like waking up from darkness.
Depression, inflammation, and what you could do
I am not a doctor, but I have been to many, so I am going to write out here the information that I have collected over the few years. The first step, if you are feeling depressed, would be going to a doctor. In Canada you can visit your family doctor if you have one, or you can go to ER. In October 2015 I was waiting for a subway train in the station and I thought of jumping under it. The thought was not spontaneous, I have been getting more and more depressed over a period of time. I told my boyfriend about my thoughts of jumping and he convinced me to go to the ER. I was terrified when the doctor who examined me said that I would be involuntarily hospitalized in the psychiatric unit. The first thing that came to mind was probably a scene from One Flew Over the Cuckoo’s Nest. Given that I was in a psychotic state, I imagined that my boyfriend and the doctors conspired to lock me up for an indefinite amount of time. Well, none of this happened. The law is that you can be involuntarily hospitalized for three days, and then your case has to be reviewed. Two opinions of physicians are required to maintain the detention.
Involuntary hospital admission – Canada
Actually I should say I got lucky that when I went to the ER I got seen by several psychiatrists and got to be examined for three days. At the moment there are not enough beds and not enough psychiatrists in Ontario, often people needing help are placed on six to nine months wait lists. Going to ER is therefore a good option because it’s more likely that there will be a psychiatrist available right away (yes, you might sit in the waiting room for five hours, but that’s not six months). Also blood tests would be performed to determine whether any health conditions could be causing your psychiatric symptoms. Tests performed could include the following:
- TSH level to check for hypo/hyperthyroidism
- Blood glucose level to check for diabetes
- Iron/ferritin levels to check for anemia
- Renal function (for chronic kidney disease)
In my experience doctors did not check for autoimmune diseases as part of the lab work, but if you are experiencing physical symptoms as well, you could ask your doctor to check this. Autoimmune testing:
- Thyroid antibody levels (Anti-Tg and Anti-TPO antibodies) – high levels can indicate Hashimoto’s thyroiditis, also Hashimoto’s Encephalopathy (but this is quite rare)
- C-reactive protein – marker of inflammation
- Antinuclear antibodies (ANA) – checking for lupus
- Rheumatoid factor – associated with rheumatoid arthritis
- Anti-NMDAR antibodies – anti-NMDA receptor encephalitis (rare occurrence)
- Celiac disease testing (it is also an autoimmune disorder)
Gastrointestinal disorders are also associated with depression. Individuals with gastritis are more likely to suffer from anxiety, panic attacks and depression. Depression and anxiety is also more often present in people with irritable bowel syndrome. If you experience any gastrointestinal/abdominal pains and discomfort, it’s important to visit a gastroenterologist. You can be tested for celiac disease. New research also indicates that many people who considered themselves having a gluten sensitivity actually had issues with high FODMAP foods. These are fermentable oligo di mono-saccharides and polyols, short chain carbohydrates and sugar alcohols. Personally I was diagnosed with chronic gastritis a few years ago, even before I got to the psychiatrist. The gastroenterologist who diagnosed me did not have any suggestions for me. A year ago I visited a different gastroenterologist, and she advised me to try a low FODMAP diet. I have been following it for a while, even after I stopped the AIP diet, and it definitely reduced my abdominal pains. Hopefully it is affecting my mood positively as well.
Gastritis linked to mood and anxiety disorders
Is gluten causing your depression
Once you talk to your family doctor or your psychiatrist about depression, if you do get diagnosed with depression, usually anti-depressants are prescribed. If you experience psychosis, anti-psychotics can be prescribed (on their own or along with anti-depressants). I am not a doctor, so it’s not for me to tell you which medication to take, but I just want to bring to your attention recent research on the link between depression and inflammation. I think no matter whether you do or don’t take psychiatric medication, it might be worthwhile to analyze your lifestyle and to think whether there are unhealthy aspects of it that you could change.
New research shows depression linked with inflammation
I know this may sound pointless – it may seem that no medication or lifestyle changes can help because it is life itself that is so meaningless, so emotionally painful, and how is that going to get changed? I used to get angry at suggestions by psychiatrists to attend therapy or my mom telling me to take fish oil. What does fish oil have to do with my life? How will it make me less lonely, how would it make life less dull and meaningless? The thought that helps me to try a suggestion is “what do I have to lose?” If I am already at the point where I no longer want to live, what will I lose by trying fish oil? Yes, it means I will agree to still be alive and try taking these stupid capsules, but I don’t have to be alive forever, it’s not possible anyways. I am not agreeing to suffer forever, I am just agreeing to stay alive for now, and to try.
Back to inflammation discussion – so for example you say “ok, fine, maybe I will try to stay alive, but so what? What is the suggestion?” Well my suggestion is in addition to discussing with your psychiatrist medication/therapy options, look into your daily diet and activities. From the article above, it is stated that the Journal of Clinical Psychiatry published a study with results indicating that increased inflammation in the body may be linked with depression. Inflammation is when there is a response from the immune system. Many different immune cells can be activated during inflammation and they produce different substances, such as antibodies (there are different types).
We need the immune system to be active to fight viruses and bacteria, but what the authors of the paper are saying, is that chronic inflammation does not help us and is damaging instead, reducing chronic inflammation may reduce depressive symptoms. PsychologyToday author in the article recommends avoiding fried foods, soda, white bread and pastries, margarine, lard, and red meat. In general highly processed foods and refined carbohydrates are considered to be linked with inflammation. White bread, white rice, pizza pops, hot dogs, salami, cookies, etc. In general a lot of doctors advise to follow a Mediterranean diet, which means reducing red meat, processed foods, refined carbohydrates and sweets. It includes eating the following:
- whole grains/pseudograins (quinoa, brown rice, millet, oats, buckwheat, etc.); it is suggested to eat them whole and not in form of grain flour
- poultry – turkey and chicken
- fish, especially fatty fish like salmon
- eggs (I suggest trying quail eggs!)
- vegetables
- berries
- olive oil instead of vegetable and seed oils
- legumes (checked whether you have issues with high FODMAP foods)
- nuts and seeds (try finding those that weren’t roasted in vegetable/seed oils, you can eat raw nuts)
- dairy – if you have issues with cow milk, there is goat milk; there is also goat yougurt and you can make goat kefir
- some fruits
I think no matter what you were diagnosed – depression, schizophrenia, bi-polar, etc., a healthy diet is very important. It’s very important for anyone. Our brain is just an organ like all other organs and it needs proper nutrients and can also get damaged, like other organs, by chronic inflammation. At first I was very skeptical about the correlation between diet and my thoughts, but then as I started experimenting with changes in what I eat, I noticed that it does affect what I think. Sometimes I am really tempted to buy ice-cream or something like that, but I just remind myself that for me it’s not worth it, it can take me to a very dark place. I just have to accept that as someone with diabetes has to watch their carb intake, I also have to watch what I eat because of my chronic autoimmune condition. This is just how it is, I have to accept that it’s chronic, and that I can’t just go to the food court and buy whatever I want. I mostly bring food from home or I buy from places that list all of their ingredients, so that I can make sure it doesn’t have gluten, cow’s dairy, a lot of sugar, high FODMAP items, etc.
Yes, it’s not pleasant having to worry about the ingredients each time you eat, but the benefit for me was a change in my thought process, and I find that the most valuable. Our thoughts and emotions are what matters because that is our experience of life, so that is the number one thing that I want to change myself, I want to have a positive life experience.