I’m not. Actually I’m pretty sure that’s not where my depression started. I am quite positive that the encephalitis – brain inflammation – had developed after several years of chronic gut inflammation. What if my irritable bowel/gastritis was stopped right after it started? What if I had known about celiac disease and stopped eating gluten not two, but ten years ago? My assumption is that I would not have developed brain inflammation then, I would not experience seeing the old women asking me to help them die, I would not feel the walls of my room closing in on me. There would be no primal fear, no encephalitis. Whatever has happened to me, happened, no point to dwell on the past, but I am writing for others, for whom such terrifying experiences may be prevented. It’s important to ask the question – are you sure your depression is only in your brain?
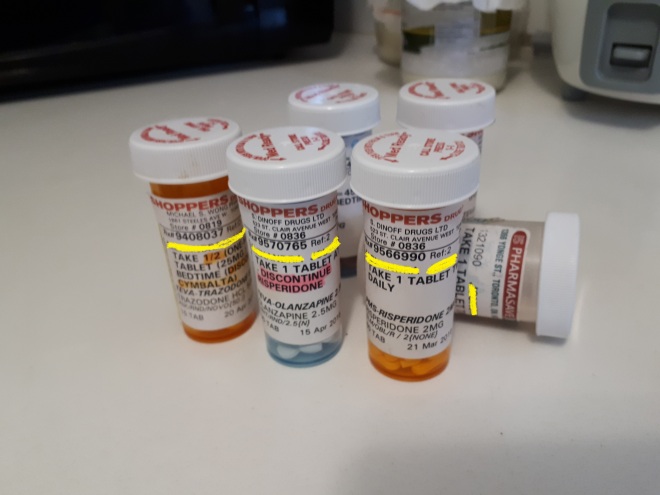
Above is my combination of the psychiatric meds that I was given by my first psychiatrist. She never questioned the origins of my depression – to her it was all a chemical imbalance in my brain, therefore she combined SSRIs, antipsychotics, benzodiazapines, and she failed at treating me. She started treating me in November 2015 and in May 2016 I bought hibachi grills and drove away into a forest with the two grills and a bag of charcoal, police had to track me. In June I could no longer work and became unemployed. Clearly I did not improve in the six months that I was her patient.
I did not improve because I don’t just have some serotonin imbalance, I have autoimmune encephalitis – brain inflammation. I also was diagnosed previously with irritable bowel syndrome (IBS) and chronic gastritis – gut inflammation. Did one lead to another? I believe so. I believe my depression started in the gut and there is research to support this theory.
“Recently, studies have emerged focusing on variations in the microbiome and the effect on various CNS disorders, including, but not limited to anxiety, depressive disorders, schizophrenia, and autism.2,8,9 Therapeutic interventions to treat dysbiosis, or disturbance in the gut, and mitigate its effects on the GBA (gut-brain axis) are only recently coming to the forefront as more is known about this unique relationship. As a result, research has been done on the use of probiotics in treatment of anxiety and depression both as standalone therapy and as adjunct to commonly prescribed medications.”
“When the human microbiome is challenged with changes in diet, stress, or antibiotics, the physiology of the normal microbiome undergoes change. A dysbiotic state leads to increased intestinal permeability and allows contents such as bacterial metabolites and molecules as well as bacteria themselves to leak through the submucosa and into the systemic circulation, a phenomenon aptly named leaky gut syndrome. … Increased intestinal permeability leads to detrimental effects on the host immune system, which have been demonstrated in diseases such as inflammatory bowel disease (IBD), diabetes, asthma, and psychiatric disorders including depression, anxiety, and autism.2,4,10,34,35“
“Depressive disorders are characterized by both neuroplastic, organizational changes, and neurochemical dysfunction.42 Illness is thought to begin when there is deregulation of these systems and can largely be attributed to cytokine release secondary to an exaggerated systemic response to stressors.39,41 Endotoxin infusions to healthy subjects with no history of depressive disorders triggered cytokine release and subsequent emergence of classical depressive symptoms. The study established a direct correlation between increased levels of IL-6 and TNF-a with symptoms of depression and anxiety,43 indicating that pro-inflammatory cytokines play a role in the development of anxiety and depression. These effects correlated with a state of chronic inflammation and altered immune cells in the peripheral blood. However, TNF-a administered to healthy subjects resulted in no depressive symptoms,38 suggesting that toxin induced inflammation caused the mood disturbance.”
Gut microbiota’s effect on mental health: The gut-brain axis
There has also been found a link between IBS and depression and recent studies are indicating that probiotics may help with both issues.
“For the new research, scientists from McMaster University in Canada recruited 44 adults with IBS as well as mild to moderate anxiety or depression. They were followed for 10 weeks; half took a daily dose of the probiotic Bifidobacterium longum, and half took a placebo. The probiotics were manufactured and provided by Nestle, which also funded the study. (Nestle was not involved in collection, analysis or interpretation of study data.)
After six weeks, twice as many people who took the probiotic had decreased depression scores compared to those who took the placebo: 64% versus 32%. Results were similar after 10 weeks, as well. When people in the study were given functional MRI scans, the researchers found that improved depression scores were associated with changes in activity of several brain areas involved in mood regulation.”
How Probiotics May Help Depression
If you are suffering from treatment resistant depression – you are not improving with the SSRIs/SNRIs/TCAs/MAOIs/NASSAs/etc., it’s important to ask yourself whether you are also suffering from any other conditions. If I had previously known all the information about the gut-brain axis, inflammation, and autoimmune diseases, it would be more evident to me that the cause of my psychiatric issues was likely gut inflammation. My severe depression started in 2015 but other health problems were starting long before that. I experienced dry and peeling skin since I was 11 years old and after the age of 12 I developed severe acne. When I was 17 I started having strong abdominal pain in the evenings. Sometimes the pain was so severe that I found it difficult to sit up. I also remember difficulties with falling asleep because as I lay down I would feel my stomach grumble and I could not relax. Later on more symptoms were added such as facial swelling, gastric pain, rapid weight gain, and brain fog. Then the depression and psychosis came. A coincidence ? Just a chemical imbalance unrelated to the other health issues? Clearly not and these symptoms were all related. They developed together as I continued to have a diet, unknowingly, that was terrible for me – pasta, bread, pizza, cheesecakes, and the symptoms declined together as I changed my diet, got treated with steroids, and started consuming fermented foods.
Now that I am equipped with all of this information I hope that I will continue to improve. I no longer have a feeling that it will only get worse and worse. I hope this will be useful to you as well and I hope I can help you feel happier again. There is more and more research now on other possible treatments for depression in addition to existing antidepressants, so I am optimistic that something will work for you, there are many things to try, don’t give up!